Optimism and Pessimism in Medicine, a viewpoint about expansion and compression of morbidity: the “Risk Compression Paradox”
Medicine is in the remarkable position of having become a victim of its own success. The number of advances in medicine are impressive, and it can save the sick from death for which there was no hope for a long time. However, together with a longer life expectancy and associated increases in chronic non-communicable diseases, this leads to higher costs and thus to the call for cutting back on medicine, because otherwise it would no longer be financially sustainable. The dilemma of modern medicine is therefore to succeed against death at the expense of an expansion of numerous diseases in people with expansion of age. Although such diseases are more and more defeatable, considerable cost issues are arising due to toxic prices for societies, such as for anti-cancer or lipid-lowering drugs.
The victorious, “plethoric” medicine inevitably creates a movement of criticism and opposition, which points to the fact that medicine is also an iatrogenic and pathogenic science. This movement increasingly and successfully criticizes the expansion of medical indications for curative and palliative procedures, but also preventive examinations and the medicalization of prevention. Such a background nourishes the irrational “cholesterol lie”-movement or the rationing movement of “smarter medicine”.
This constantly evolving pessimism towards medicine finds its reason also in an increasing disenchantment with the art of medicine and its pandemic spread viewed as an anti-romantic invasion into the privacy of the natural individual human being. By consequence, rejection attitudes regarding influenza vaccine, but also fundamental rejection of medical services such as palliative medicine replaced by advocacies for voluntary death using Pentobarbital (Exit movement in Switzerland). Such movements fit well with the utilitarian viewpoint: no waste of limited resources. At the same time, in the economization of society, the productive value of humans is used to decide about withholding costly interventions, concealed behind economical calculations about quality adjusted life years (QALY). The acceptance of the finiteness (“Why I Hope to Die at 75”1) by the biomedical ethicist Ezechiel Emanuel and the rationing demand for medical services as an economic victory against medicine are a logical consequence.
The perception of medicine as a failure of success was published by Ernest M. Gruenberg in a relentless report by Milbank Quarterly in 19772. His early discussion regarding senile brain disease is also impressive in view of the current situation with the accumulation of senile dementia. As a result, he declared the failure of medicine, because it leads to disease expansion.
Today’s medicine has an immense knowledge of the effectiveness of prevention. However, there are problems with its application. Refusal to medicalize a life with preventive pills is a common skeptical and pessimistic attitude, where side effects of preventive therapies are purposely exaggerated and beneficial effects neglected, eventually by the aid of a conspiracy of the pharmaceutical industry against mankind.
Medicine inevitably leads to more medicine and more morbidity, because it needs diseases to gain new insights. An extinction of morbidity is poison for medical progress. The ultimate medical victory over diseases must generate an expansion of morbidity in order to maintain the cybernetic learning system that makes this goal achievable. The situation is thus hopeless and confirms a pessimistic attitude towards medicine.
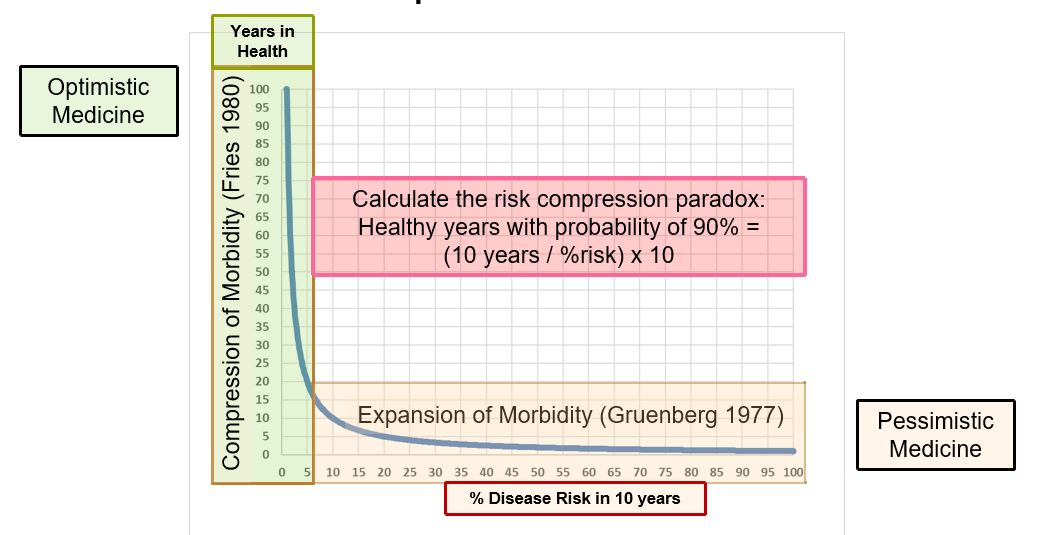
The optimists see it completely differently. They want to push back the diseases until natural death occurs. Prevention does no harm and is a prerequisite for keeping people healthy. This concept was formulated in 1980 by James Fries3 and has been recently substantively verified using a 40-year observation: individuals 40 years later with a favorable risk profile for cardiovascular disease had an absolute effect of compression of morbidity and associated costs4.
There is a simple mathematical relationship between risk and healthy life expectancy, that will have enormous implications for preventive medicine, because it indicates, where the camp of pessimists and optimists separate. We term our observation the “risk compression paradox”, which can simply be calculated by “healthy years with probability of 90% = 10 years / (%risk x 10)”. As can be seen in the central figure, a high (90%) probability to gain healthy years has an exponential appearance, once risk is below 5% in 10 years. The expansion of healthy years at the expense of compression of morbidity is extremely high, when we lower low risk even further (e.g. from 7% to 2% with a gain of 36 years), whereas in persons with higher risk, same amounts of absolute risk reduction will not increase the probability to remain healthy but for a few years.
Conviction, education, financing and encouragement will increase the effectiveness of preventive medicine, resulting in a shift from disease expansion to disease compression. The solution of the conundrum of a failing medicine, which creates diseases in increasingly viable humans lies in the optimistic answer towards a maximized prevention. This will weaken the skills of future medicine, because it will lose many patients. However, the solution of those who believe that prevention is falsified, want to ration prevention, and are caught up in a problematic concept of natural life causes the expansion of morbidity they claim to prevent. The pessimism in medicine is just generating the expansion of morbidity she warns of and is nothing less than a self-fulfilling prophecy. The optimists’ strategy, accomplishes its goal by rationally applying medical knowledge using proven efficiency of prevention in order to compress morbidity in an increasingly healthy and productive society.
The conundrum of the failure of medicine despite all its successes has found its solution. Public Health has to focus on perfecting evidence-based prevention, elimination of anti-preventive irrational and scientifically unsustainable pseudo-falsifications and to create a climate of trust into the strengths of preventive medicine.
References:
- Emanuel E. Why I hope to die at 75 [Internet]. Atl. 2014;Available from: http://www.theatlantic.com/magazine/archive/2014/10/why-i-hope-to-die-at-75/379329/
- Gruenberg EM. The Failures of Success. Milbank Mem. Fund Q. [Internet]. 1977;55:3–24. Available from: www.ncbi.nlm.nih.gov/pmc/articles/PMC2690285/pdf/milq0083-0400.pdf
- Fries J. Aging, natural death, and the compression of morbidity. N Engl J Med. 1980;303:130–5.
- Allen NB, Zhao L, Liu L, Daviglus M, Liu K, Fries J, et al. Favorable Cardiovascular Health, Compression of Morbidity, and Healthcare CostsClinical Perspective. Circulation. 2017;135:1693–1701.
This is a scientific website of the vascular risk foundation. In an aging population, the compression of morbidity towards the end of life is achievable, when control of risk factors in middle age is favorable. The magnitude of such effects is the key research object in our population of 5’352 healthy subjects from Germany and Switzerland.
This website is in preparation. The german website is available with the key informations here.